Dr. Taly Gilat-Schmidt makes advancements in artifact reduction and radiation-dose-tracking technologies
May 26, 2021
A professor of Biomedical Engineering at the Marquette University and Medical College of Wisconsin Joint Department of Biomedical Engineering, Dr. Taly Gilat-Schmidt has dedicated her life to her love of medical imaging systems. Balancing a dynamic load of teaching, writing and research activities, Dr. Gilat-Schmidt’s interests range from imaging physics to image reconstruction and deep learning. With particular expertise in the field of computed tomography, her recent work on radiation dose tracking may prove her most immediate opportunity to satisfy her ultimate goal—improving patient care.
From complex bone fractures to internal injuries, and especially critical in cancer treatment, computerized tomography (CT) scans have been instrumental in healthcare for half a century. These scans use computers and moving x-rays that can create cross-sectional images of the body, showing more detail than a regular x-ray. A CT scan can be administered to any part of the body and uses computer processing to create detailed imaging of the bones, blood vessels and soft tissues. CT scans are widely used because they are quick, completely painless, and—most importantly—very accurate.
 Far outweighed by the benefits of early disease detection and routine care and diagnostics, as with so many good things, CT scans do have their drawbacks. Like other forms of x-rays, CT scans cause atoms to release energy in the form of radiation, and a person exposed to this radiation repeatedly or in very large amounts may suffer damage to their DNA, which in turn increases their risk of developing cancer. While a patient’s response to various radiation doses is as unique as the individual themselves, until very recently, CT radiation dosage was difficult to measure or predict, making it difficult to determine how much radiation exposure was too much, or even how much exposure a particular person or organ system might have received. As a result, a push for improved imaging quality and patient safety in scanning has been the focus of many institutions, nationwide, for well over a decade.
Far outweighed by the benefits of early disease detection and routine care and diagnostics, as with so many good things, CT scans do have their drawbacks. Like other forms of x-rays, CT scans cause atoms to release energy in the form of radiation, and a person exposed to this radiation repeatedly or in very large amounts may suffer damage to their DNA, which in turn increases their risk of developing cancer. While a patient’s response to various radiation doses is as unique as the individual themselves, until very recently, CT radiation dosage was difficult to measure or predict, making it difficult to determine how much radiation exposure was too much, or even how much exposure a particular person or organ system might have received. As a result, a push for improved imaging quality and patient safety in scanning has been the focus of many institutions, nationwide, for well over a decade.
Sporting funding from two grants from the National Institutes of Health and a separate award from GE Healthcare, recent work of Dr. Gilat-Schmidt and her Medical Imaging Systems Laboratory seeks to satisfy these exact aims:
Over the past decade, there has been development in x-ray detectors that give spectral information, so you at least have more information about what energy that x-ray was. My lab has been working for over ten years on understanding how we extract the information—how we use it to improve the images.
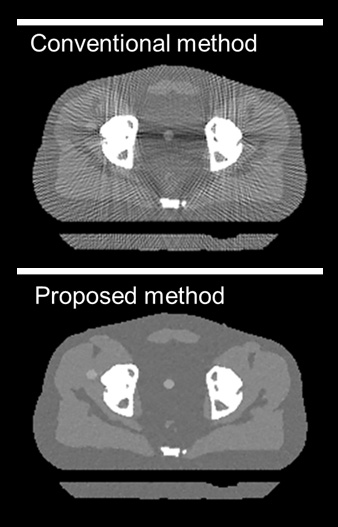
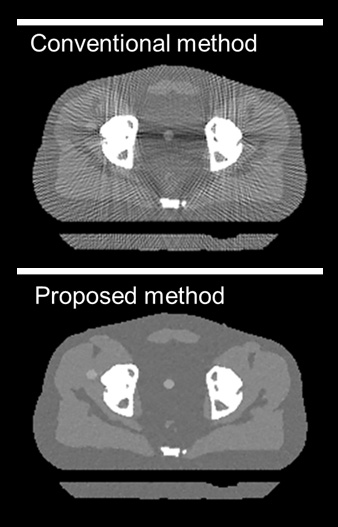
As an example, MISL is working to improve how CT technology highlights contrast between different bodily tissues and to reduce “artifacts” or “degradations”—stray markings that can occur when a person has materials like metal in their body. These types of flaws in scanning are met with advanced computer algorithms that use the newly acquired spectral information to infer accurate anatomies when images are reconstructed. When image quality improves and produces a picture free from artifact, doctors are able to better plan radiation therapies and work with their patients to make clearer, more tailored treatment plans.
MISL’s work in improving the quality and safety of CT imaging is especially important when considering the treatment of cancer in children who, when exposed to radiation earlier in life, could have a greater chance of developing cancer much later into adulthood. To approach this, MISL has partnered with Children’s Hospital of Wisconsin and Varian Medical Systems to direct efforts in understanding radiation exposure to our youngest patients.
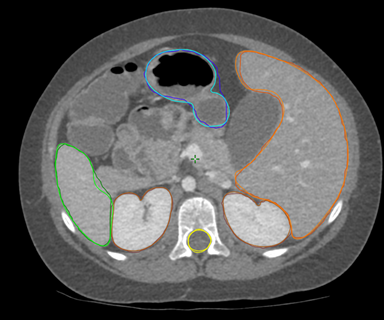 Focusing specifically on the chest, abdomen, and pelvis, the project uses deep-learning technology to train computers to identify the organs imaged in each CT scan and record the radiation deposited in the body, deepening our understanding of how much radiation each organ is receiving per scan. These two points have been evaluated independently—including an extensive computational and experimental validation by MCW postdoc Sara Principi—and the project now has amassed a database of 360 pediatric CT scans, which will be used to estimate the radiation dose using their tool, as compared to the industry standard. With good training data on correctly locating a patient’s organs, this process could then be tailored to identify other parts of the body, such as the brain.
Focusing specifically on the chest, abdomen, and pelvis, the project uses deep-learning technology to train computers to identify the organs imaged in each CT scan and record the radiation deposited in the body, deepening our understanding of how much radiation each organ is receiving per scan. These two points have been evaluated independently—including an extensive computational and experimental validation by MCW postdoc Sara Principi—and the project now has amassed a database of 360 pediatric CT scans, which will be used to estimate the radiation dose using their tool, as compared to the industry standard. With good training data on correctly locating a patient’s organs, this process could then be tailored to identify other parts of the body, such as the brain.
Whenever I teach an imaging class or teach a module on imaging for the freshman, I always start with an image and say, ‘See! This is amazing! Look! You can see inside of a person without cutting them open!’ It’s just amazing. It just has always fascinated me. I couldn’t imagine studying anything else.
At the end of the day, whether in the office, the classroom or the lab, the goal of faculty member Dr. Gilat-Schmidt and her Medical Imaging Systems Laboratory remains the same: improve patient outcomes. And while Dr. Gilat-Schmidt's current work enables her to directly approach the care of individuals—and particularly children—undergoing repeated CT exposures and radiation therapy, certainly the implications and potential applications of the radiation dose tracking project reach much further. More accurate information regarding estimated CT dosing could potentially be tracked over a lifetime and be used to improve our understanding of radiation risk and to improve our design of CT acquisition methods. As with most scientific endeavors, the path to completion is long, but Dr. Gilat-Schmidt remains invigorated by her passion for medical imaging systems, which she describes as an elegant combination of physics, algorithms and math.
View more BME News

 Far outweighed by the benefits of early disease detection and routine care and diagnostics, as with so many good things, CT scans do have their drawbacks. Like other forms of x-rays, CT scans cause atoms to release energy in the form of radiation, and a person exposed to this radiation repeatedly or in very large amounts may suffer damage to their DNA, which in turn increases their risk of developing cancer. While a patient’s response to various radiation doses is as unique as the individual themselves, until very recently, CT radiation dosage was difficult to measure or predict, making it difficult to determine how much radiation exposure was too much, or even how much exposure a particular person or organ system might have received. As a result, a push for improved imaging quality and patient safety in scanning has been the focus of many institutions, nationwide, for well over a decade.
Far outweighed by the benefits of early disease detection and routine care and diagnostics, as with so many good things, CT scans do have their drawbacks. Like other forms of x-rays, CT scans cause atoms to release energy in the form of radiation, and a person exposed to this radiation repeatedly or in very large amounts may suffer damage to their DNA, which in turn increases their risk of developing cancer. While a patient’s response to various radiation doses is as unique as the individual themselves, until very recently, CT radiation dosage was difficult to measure or predict, making it difficult to determine how much radiation exposure was too much, or even how much exposure a particular person or organ system might have received. As a result, a push for improved imaging quality and patient safety in scanning has been the focus of many institutions, nationwide, for well over a decade.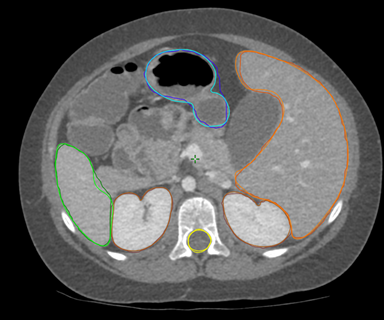 Focusing specifically on the chest, abdomen, and pelvis, the project uses deep-learning technology to train computers to identify the organs imaged in each CT scan and record the radiation deposited in the body, deepening our understanding of how much radiation each organ is receiving per scan. These two points have been evaluated independently—including an extensive computational and experimental validation by MCW postdoc Sara Principi—and the project now has amassed a database of 360 pediatric CT scans, which will be used to estimate the radiation dose using their tool, as compared to the industry standard. With good training data on correctly locating a patient’s organs, this process could then be tailored to identify other parts of the body, such as the brain.
Focusing specifically on the chest, abdomen, and pelvis, the project uses deep-learning technology to train computers to identify the organs imaged in each CT scan and record the radiation deposited in the body, deepening our understanding of how much radiation each organ is receiving per scan. These two points have been evaluated independently—including an extensive computational and experimental validation by MCW postdoc Sara Principi—and the project now has amassed a database of 360 pediatric CT scans, which will be used to estimate the radiation dose using their tool, as compared to the industry standard. With good training data on correctly locating a patient’s organs, this process could then be tailored to identify other parts of the body, such as the brain.